Four ways funders can support better health services in low-income countries
Read this post in French here.
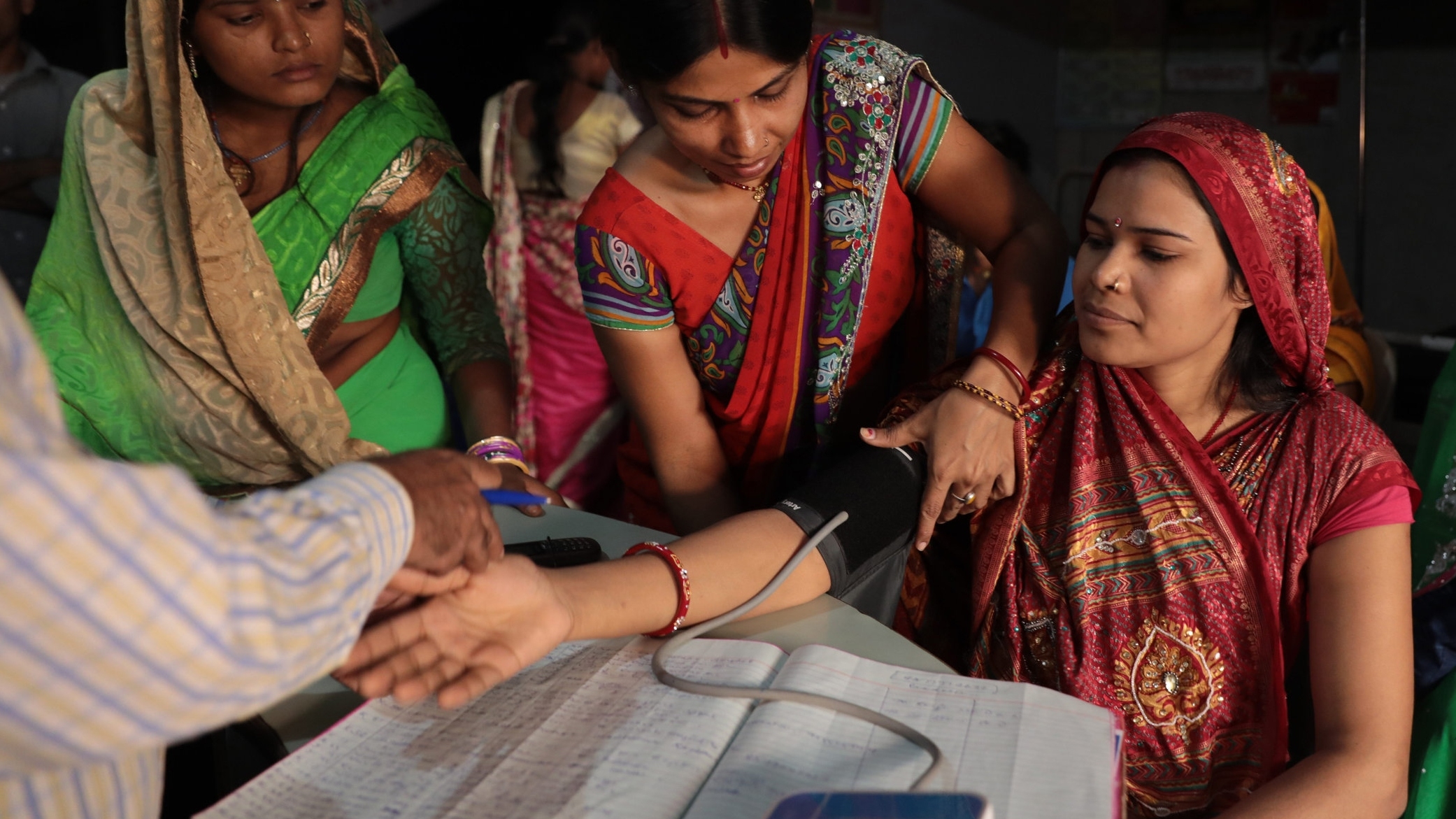
Today, civil society organizations around the world are marking Universal Health Coverage Day by working together to raise awareness about an important commitment more and more governments are making: that all people have access to the health services they need, without falling into financial hardship paying for them, otherwise known as universal health coverage (UHC). Many of the organizations we support are working to create more equitable and better quality health services in low-income countries. They’re thinking about how universal health coverage might help those who often go without or receive the poorest quality health services: women, children, people with disabilities, and informal workers who lack financial protections.
While I’m thrilled to see the energy and momentum of this global advocacy day, funders like us can do more to support education, community organizing ,and feedback mechanisms, like this seminar for journalists in Pakistan and this town hall meeting in Nigeria. Today, as people from Karachi to Abuja ask their governments to commit more money to improve people’s health, it’s also a good day for funders to consider what else we can do the remaining 364 days of the year.
The universal health coverage advocates I’ve spoken to in the United States, Europe, Kenya, Senegal, Guatemala and India say that platforms like UHC2030 reinforce political will and create important channels for civil society voices from lower- and middle-income countries. They help inform the World Bank and International Monetary Fund about the realities in low- and middle-income countries, and officials from those multilateral institutions may then help shape their partner governments’ policies. UHC2030 also links these advocates with others across the globe so they can learn from each other. And partnerships like the Global Financing Facility for Every Woman Every Child (GFF) help funders, policymakers, health providers, and people work together toward achieving the vision of universal health coverage.
Still, global advocacy campaigns and platforms are not enough. Much more is needed, especially to support efforts within countries throughout the rest of the year. These are the four ways universal health coverage advocates have told me we—and other funders—can help:
1. Get more resources where it counts the most.
National and sub-national coalitions of civil society and advocacy organizations, human rights activists, patients’ groups, professional associations, women’s rights networks, and others who care deeply about health need more support to get basic information about when and how policy decisions are made, including what and who gets covered in essential benefits packages, the financial protections that will be put into place to ensure equity, how universal health coverage gets financed and how resources are allocated from national to sub-national levels. Funders could invest more in efforts to organize and build the capacity of such coalitions to gain access to and share information in a more timely way, secure a seat at decision-making tables, and put into place performance monitoring and citizen feedback mechanisms.
For example, in East Africa, PATH, with support from the Bill and Melinda Gates Foundation, is holding a series of thought-provoking Accountability Learning Labs to enable health advocates, government officials, and development partners from across the region to come together in a safe space, to analyze the gap between governments’ commitments for improved healthcare and the reality. They are sharing practical solutions for how they can work most effectively together to advance universal health coverage. The labs will promote multi-stakeholder engagement, joint learning and smarter advocacy strategies in response to their particular country dynamics, such as decentralized health systems.
2. Ensure that those most affected and least heard from are able to participate.
In low- and middle-income countries, women are the primary users of health services and most often the least likely to have financial protection. It’s critical to ensure that women’s rights organizations, national federations of people with disabilities and other groups that understand the needs of these important universal health coverage constituencies are well-informed, able to offer feedback, and have a seat at the table as decisions are being made.
In West Africa, we recently approved a grant to CICODEV, a Senegalese NGO that provides consumers with information about the services that they should expect to receive from their local health facility and what they can do about it if their experience does not match those expectations. CICODEV trains citizen volunteers to raise awareness and monitor the quality of care at their local health facilities, especially related to Senegal’s commitment to provide maternal and child health services free of charge. CICODEV then uses the information gathered from its “citizen observatories” in its national advocacy work. Amadou Kanoute, CICODEV’s executive director describes it this way:
“A mismatch between vision and program delivery is the worst thing that can happen to a leader. In public health, the effects can be especially disastrous since good health is a crucial catalyzer for socio-economic development. At CICODEV, we believe collecting information on how well health services are being delivered (as perceived and lived by citizens), and then pushing that information up to decision makers and duty bearers decreases the risk of policy failure. And that’s what we are doing!”
You can read more about Mr. Kanoute’s story here.
3. Support country-based analytical work and open access to global public goods.
The availability and capacity to use evidence should follow international principles, such as Sustainable Development Goal 17 to enable better planning, implementation, and accountability for universal health coverage. Importantly, this work should examine who may be left behind, and what it will take to achieve full coverage and financial protection for these groups. Funders can help ensure that materials produced are also made available in ways that are relevant, understandable, and actionable at the country level and through regional learning networks.
Many pointed to the Joint Learning Network as an effective way for policymakers across countries to identify gaps and share approaches for better use of evidence in decision making at the country level. Earlier this year, our Evidence-Informed Policymaking program made a grant to the Africa Centre for Systematic Reviews and Knowledge Translation at Makerere University in Uganda to offer policymakers faced with time-sensitive decisions “rapid response” syntheses of relevant research. This program builds on the center’s track record of informing prior Ministry of Health decisions. We are looking forward to seeing to what extent they and other rapid response producers expand this service and whether it influences how other research organizations engage with governments.
Two good examples of global public goods are the World Bank’s Service Delivery Indicators for health and education, which have amassed comparable data from health facilities in several countries in Africa that can be used to better understand the quality of services that people are actually receiving; and the International Initiative for Impact Evaluation’s evidence map gaps and more than 400 systematic reviews related to health.
4. Ensure civil society and research organizations from low- and middle-income countries have meaningful input and are part of the dialogue around the UN High-Level Meeting on Universal Health Coverage in 2019.
Funders could provide support for research, background papers, and country-level consultations that bring new perspectives and voices to the conversation in the lead-up to the meeting. Funders could also provide travel grants for a more robust representation from civil society in September through platforms like the UHC 2030 Civil Society Engagement Mechanism.
What do we plan to do?
In 2019, we plan to pursue a few targeted grantmaking opportunities for advancing citizen engagement and government accountability for UHC under our existing Transparency, Participation, and Accountability program strategy. We are especially interested in places where universal health coverage policies are well underway, and where there are civil society organizations that are ready to play a leadership role, such as Kenya, Uganda, Senegal, Burkina Faso and Ghana. Our aim is to catalyze other investments, both domestic and international. This is not a new initiative or line of grantmaking for us, but rather will be part of how we go about implementing our service delivery monitoring sub-strategy, which focuses on these questions across health, education, water, and sanitation services.
Finally, my colleagues and I plan to share updates about what we are funding and what we and our grantees are learning in future blogs and on social media (@Hewlett_Found and @pscheid6). What else do you think we, and other funders, can do? We will welcome your feedback and ideas!


